Rheumatoid arthritis (RA) is an autoimmune disease driven by chronic, systemic inflammation that damages synovial joints. Medications like methotrexate, biologics, and JAK inhibitors remain the standard of care. Supplements can sometimes help with symptoms or medication needs—but they won’t replace DMARDs. This guide cuts through the noise with three buckets:
- Promising / Adjuncts with Human Evidence
- Hyped or Questionable
- Likely Worthless (for RA) or Too Risky
You’ll also find realistic dosages, quality cues, and drug-interaction red flags.
This article may contain affiliate links. If you click through and buy, we may earn a small commission at no extra cost to you.
1) Promising / Adjuncts with Human Evidence
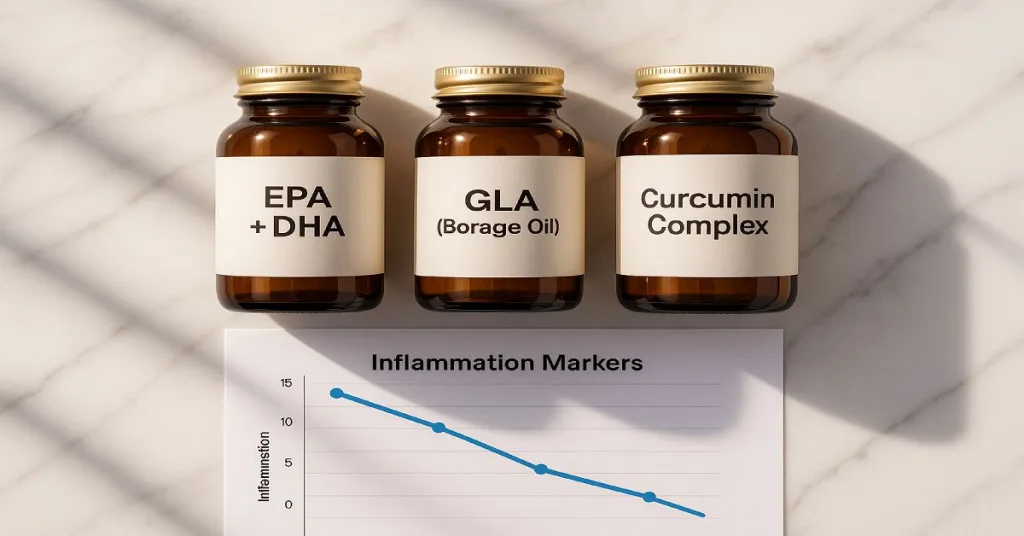
Omega-3s (EPA + DHA from fish oil)
Why it’s here: Multiple human studies show modest improvements in RA pain, stiffness, tender or swollen joints, and reduced NSAID use when doses are high enough. Omega-3 fatty acids are among the most researched rheumatoid arthritis supplements for reducing inflammation.
Typical dose: 2–3 g/day combined EPA + DHA (check the label for actual EPA + DHA, not just “fish oil”).
Notes/risks: Can increase bleeding risk at higher intakes; monitor if you’re on anticoagulants.
Gamma-Linolenic Acid (GLA) from Borage, Evening Primrose, or Black Currant
Why it’s here: Several well-done trials show meaningful reductions in RA signs and symptoms with adequate GLA intake, especially from borage oil.
Typical dose: Around 1.4 g GLA/day (often achieved with borage oil).
Notes/risks: Choose PA-free products. May cause mild GI upset.
Curcumin (Turmeric Extract)
Why it’s here: Clinical data in inflammatory arthritis show reductions in CRP and symptom scores with standardized curcumin. Bioavailability-enhanced forms perform best.
Typical dose: 500–1000 mg/day of a bioavailability-enhanced extract (with piperine or phospholipids).
Notes/risks: Possible interaction with anticoagulants; can irritate the stomach at high dose.
Vitamin D (only if low)
Why it’s here: Many RA patients have low vitamin D; correcting deficiency may modestly improve pain or disease activity.
Typical dose: 800–2000 IU/day for maintenance; 4000 IU/day is within the tolerable upper limit for short-term correction.
Notes/risks: Monitor blood levels and calcium to avoid toxicity.
Probiotics / Gut-Targeted Adjuncts
Why it’s here: The microbiome influences immune signaling. Small trials show modest reductions in disease activity and CRP, though results are inconsistent.
Typical dose: 10⁹–10¹⁰ CFU/day for 8–12 weeks using Lactobacillus or Bifidobacterium strains.
Notes/risks: Early evidence only; discontinue if no benefit after a few months.
2) Hyped or Questionable for RA
These may help osteoarthritis (OA), but RA-specific evidence is weak.
Glucosamine + Chondroitin
Evidence: Large OA studies are mixed; for RA there’s no convincing benefit.
Typical dose: Glucosamine sulfate 1500 mg/day + Chondroitin 800–1200 mg/day.
Notes/risks: May affect glucose control or warfarin. Sulfate form preferred over HCl.
Collagen
Evidence: Undenatured Type II (UC-II) at 40 mg/day shows some OA benefit; RA evidence is inconclusive. Hydrolyzed collagen targets OA and skin.
Verdict: Helpful for OA, not RA.
Eggshell Membrane (NEM)
Evidence: Improves knee OA symptoms at 500 mg/day. No RA trials exist.
Verdict: OA-only; likely irrelevant for RA.
Boswellia serrata (AKBA extract)
Evidence: Anti-inflammatory and OA-positive, but RA data are minimal.
Typical dose: 300–500 mg extract 2–3×/day (30–40 % boswellic acids, 5–10 % AKBA).
Verdict: Promising botanical, not well-proven for RA.
MSM (Methylsulfonylmethane)
Evidence: Small OA trials show relief at 3 g twice daily; no RA studies.
Verdict: Probably irrelevant for RA.
Avocado/Soybean Unsaponifiables (ASU)
Evidence: OA studies show reduced pain and possible structure benefit; none for RA.
Verdict: OA-focused, not RA.
Tamarind-Based Joint Blends
Evidence: Knee OA studies report quick pain relief; no RA trials.
Verdict: Interesting botanical, unproven for RA.

3) Likely Worthless or Too Risky
- Glucosamine/Chondroitin for RA: No measurable benefit.
- SAM-e (S-adenosyl-L-methionine): OA pain data only; interacts with antidepressants.
- Thunder God Vine (Tripterygium wilfordii): Potent immunosuppressant with serious toxicity—avoid.
- Oral Arnica, Chaparral, Red Yeast Rice: Unsafe or irrelevant for RA.
Practical Dosing & Quality Summary
| Supplement | Typical Daily Dose | Notes |
|---|---|---|
| Omega-3 (EPA + DHA) | 2–3 g combined | Enteric-coated; third-party tested |
| GLA (Borage Oil) | 1.4 g GLA | Verify PA-free certification |
| Curcumin (enhanced) | 500–1000 mg | Take with food or oil |
| Vitamin D | 800–2000 IU (maintenance) | Test and adjust by labs |
| Probiotics | 10⁹–10¹⁰ CFU 8–12 weeks | Evaluate benefit after 2–3 months |
What Actually Moves the Needle
- Medication adherence: DMARDs and biologics remain essential. Supplements can only complement them.
- Correct deficiencies: Vitamin D, iron, or others if confirmed low.
- Anti-inflammatory diet: Fatty fish, olive oil, colorful produce.
- Quality control: Look for NSF, USP, or IFOS certification.
- Track outcomes: Log stiffness minutes, tender joint counts, NSAID use.
Interaction & Safety Watch-Outs
- Bleeding risk: Fish oil, curcumin, and GLA.
- Immunosuppression overlap: Botanicals plus biologics = infection risk.
- Liver/Kidney strain: Overlapping “joint blends” or high-dose herbs.
- Allergies: Fish, soy, avocado, egg, seed oils.
- Pregnancy: Avoid non-essential botanicals unless cleared.
Verdict
Best-supported adjuncts
- Omega-3 EPA + DHA (2–3 g/day)
- GLA (from borage or primrose) (~1.4 g/day)
- Curcumin (500–1000 mg/day enhanced)
- Vitamin D (if low)
- Probiotics (trial basis)
Questionable or OA-specific
- Glucosamine/Chondroitin
- Collagen / UC-II
- Eggshell Membrane
- Boswellia
- MSM
- ASU
- Tamarind blends
Avoid
- SAM-e (for RA)
- Thunder God Vine (too toxic)
- Oral Arnica / Chaparral / Red Yeast Rice
Building a Smart RA Supplement Plan
- Confirm diagnosis and stay on prescribed meds.
- Check labs—especially vitamin D.
- Add one evidence-based supplement at a time.
- Evaluate after 8–12 weeks.
- Keep what helps; drop what doesn’t.
- Avoid “everything in one” blends with fairy-dust doses.
This content is for informational purposes only and is not intended as medical advice. Always consult with your healthcare provider before starting any new supplement or treatment.
for further reading: Fish Oil Supplements: Hype vs Reality, Plus Smarter Alternatives
📚 Sources
- Long-Term Effect of Omega-3 Fatty Acid Supplementation in Active Rheumatoid Arthritis: A 12-Month, Double-Blind, Controlled Study — PubMed
- Effects of Curcumin Supplementation on Inflammatory Biomarkers in Patients with Rheumatoid Arthritis and Ulcerative Colitis: A Systematic Review and Meta-Analysis — ScienceDirect
- Eggshell Membrane in the Treatment of Pain and Stiffness from Osteoarthritis of the Knee: A Randomized, Multicenter, Double-Blind, Placebo-Controlled Clinical Study — PubMed Central
- The Best & Worst Foods for Your Joints — EatingWell
- Can Vitamin D Supplements Prevent Autoimmune Disease? — Harvard Health Publishing