Is GERD Really Caused by a Vitamin Deficiency? What the Science — and My Recovery — Suggests
GERD vitamin deficiency is one of the most overlooked causes of chronic reflux, especially in people who’ve been on acid blockers for years. Millions of people are living with GERD, or gastroesophageal reflux disease — a chronic condition that causes acid to back up into the esophagus, triggering heartburn, coughing, nausea, chest tightness, and disrupted sleep. The standard medical answer is to prescribe proton pump inhibitors (PPIs) like pantoprazole, omeprazole, or esomeprazole — drugs designed to shut down stomach acid production.
But what if GERD isn’t actually caused by too much stomach acid?
What if, for some people, it’s caused by a deeper issue — something that PPIs only make worse?
New research suggests that vitamin and mineral deficiencies may play a significant role in both causing and worsening GERD — and that long-term use of acid-reducing medication might be feeding a cycle that keeps people sick.
This post may contain affiliate links. If you click and buy, we may earn a small commission at no extra cost to you. Thank you for supporting the site.
What Happens When You Shut Off Acid Too Long?
PPIs are incredibly effective at reducing acid. That’s their job. But stomach acid isn’t just there to cause heartburn — it’s essential for digestion.
You need strong stomach acid to:
- Break down protein
- Absorb calcium, magnesium, iron, and zinc
- Unlock vitamin B12 from food
- Trigger bile flow and pancreatic enzyme release
- Kill off harmful bacteria and pathogens
So what happens when you block acid for months or years? You don’t digest food properly. You don’t absorb nutrients. And your digestive system slowly becomes less efficient and more inflamed.
In long-term PPI users, studies have shown clear drops in:
- Magnesium
- Vitamin B12
- Iron
- Zinc
- Folate
- Calcium
- Vitamin C
Some of these are essential for muscle tone, including the sphincter that keeps stomach acid where it belongs. Others affect gut lining repair, nerve function, and inflammation control — all of which can influence reflux symptoms.
Is Low Stomach Acid More Common Than We Think?
Ironically, many people diagnosed with GERD may not have high acid at all — they may have low acid.
Low stomach acid (hypochlorhydria) can cause:
- Bloating
- Belching
- Reflux (due to poor digestion and delayed stomach emptying)
- Bad breath
- Constipation or diarrhea
- Nutrient malabsorption
This happens more often as we age. And it’s made worse by long-term PPI use.
So when a doctor says, “You’re having heartburn — take this to reduce acid,” it might actually be the exact wrong move for people whose digestion is already compromised.
How Nutrient Deficiencies Could Be Driving GERD
Let’s look at the evidence behind a few key nutrients and how they relate to reflux.
1. Magnesium
Magnesium is crucial for muscle function, including the lower esophageal sphincter (LES) — the valve that separates the stomach from the esophagus. If it weakens or relaxes at the wrong time, acid escapes upward.
Low magnesium levels can also cause cramping, nausea, fatigue, and anxiety — all common complaints in long-term GERD sufferers. PPIs are known to reduce magnesium absorption over time, and several case studies link magnesium repletion to symptom relief in patients with chronic reflux.
2. Vitamin B12
B12 absorption depends on stomach acid and intrinsic factor, both of which are reduced by PPI use. B12 deficiency can lead to fatigue, nerve issues, and possibly even esophageal dysfunction. In one study, over 50% of long-term PPI users were found to have suboptimal B12 levels.
3. Iron and Zinc
Both minerals require stomach acid for proper absorption. Iron deficiency can lead to anemia and fatigue. Zinc is critical for tissue repair — including the lining of the esophagus and stomach — and for immune function. Zinc deficiency may also contribute to delayed wound healing and inflammation in the gut.
4. Vitamin D and Calcium
These are more indirect but still relevant. Low stomach acid may reduce calcium absorption, which combined with low vitamin D can lead to bone loss. Poor posture and reduced muscle tone from musculoskeletal issues may worsen GERD symptoms in some individuals.
5. Glutathione and Antioxidants
Oxidative stress in the esophagus contributes to chronic inflammation. Nutrients like NAC (which helps make glutathione), vitamin C, and CoQ10 can help buffer that damage — but again, absorption depends heavily on proper digestive function.
Real-World Example: What Happened When I Quit Pantoprazole
I’m not a doctor. I didn’t set out to experiment on myself. But after years on pantoprazole, I found out I had multiple vitamin and mineral deficiencies — and it wasn’t just on paper. I felt it. My energy was wrecked. My digestion was a mess. And worst of all, my heart began showing signs of weakness.
Pantoprazole didn’t fix my GERD. It numbed the symptoms while draining my body of what it needed to function. I stopped taking it. Cold turkey. The rebound acid was hell, but I knew I couldn’t go back.
I started supporting my body instead.
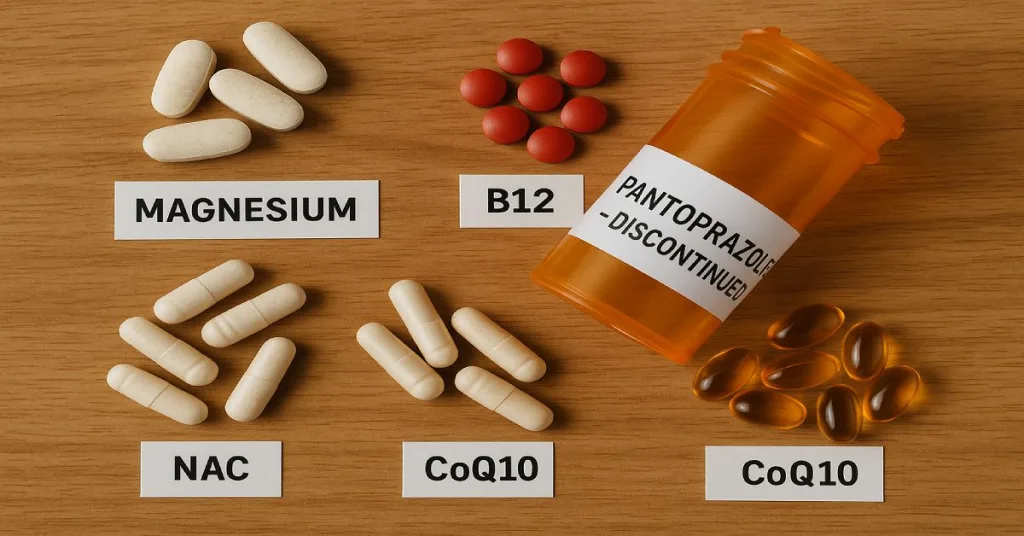
Here’s what I added — one supplement at a time — and what actually seemed to help as I rebuilt my digestion.
Magnesium (Vitalitown Complex)
Started for heart health. But within weeks, the bloating and pressure in my chest eased up. Digestion became more regular. I later found studies confirming that magnesium deficiency affects the esophageal valve. I believe this was one of the biggest turning points.
Taurine (NOW Foods)
Known for cardiovascular support, taurine also helps with bile acid formation and fluid regulation in the gut. After adding it, I noticed meals sat better. No more heavy, greasy after-meal regret. Fats digested more cleanly.
NAC (N-Acetyl Cysteine)
This one supports glutathione production, your body’s master antioxidant. It helps the liver, lungs, and the gut lining. My inflammation dropped. No more raw, burned feeling in the throat after eating.
Life Extension Two-Per-Day
This isn’t a typical multivitamin. It includes active forms of B12, folate, and high doses of other critical nutrients. I didn’t want to guess which deficiencies I had — I just wanted to cover the base. And it worked.
CoQ10, L-Carnitine, and D-Ribose
These weren’t digestive supplements per se — they were added for heart health. But I started noticing indirect improvements in energy after meals, better appetite regulation, and more consistent digestion. The connection between mitochondria and gut repair is real.
What I Removed
I also cut out a few things that weren’t helping — namely cinnamon. Some people swear by it for digestion. Not me. It seemed to worsen the burning. Once I stopped, I felt better within a few days.
The Bigger Picture: GERD Isn’t Just About Acid
If you’re dealing with GERD, ask yourself this:
- Are you treating a symptom or the cause?
- Has your medication helped long-term, or just masked discomfort while your health declines?
- Have you tested your nutrient levels?
- Is your digestion actually working — or are you just suppressing what your body is trying to signal?
It’s not about quitting meds recklessly. But if acid blockers are causing deficiencies, and those deficiencies are fueling the very symptoms they’re supposed to stop… that’s a problem.
What to Do if You Suspect a Deficiency
If you’ve been on a PPI for a long time:
- Get your magnesium, B12, and iron tested
- Ask your doctor about tapering options
- Start a high-quality multivitamin
- Consider adding a magnesium supplement
- Track how you feel after meals
- Remove any supplements or foods that worsen your symptoms
Rebuilding your gut takes time. I didn’t feel better in a week. But a few months in, the difference was night and day.
Conclusion: GERD Might Not Be What You Think It Is
The idea that GERD is caused by too much acid is outdated. In many cases, it’s the opposite — poor digestion, low acid, and chronic nutrient deficiencies that spiral into inflammation and dysfunction.
PPIs are a short-term crutch, not a long-term solution. If you’ve been stuck on them for years, and nothing’s getting better, it may be time to rethink the entire approach.
In my case, once I stopped blocking acid and started rebuilding my body with the nutrients it was missing, the reflux faded.
Not managed.
Not masked.
Gone.
see also: N-Acetyl Cysteine (NAC): The Antioxidant That Does More Than You Think